Written and medically reviewed by Rich LaFountain, PhD
By: Rich LaFountain
A lot of people have been asking us about how fasting might intersect with COVID-19 risk, infection, and the vaccine. In this brief article we’re hoping to provide some evidence-based clarity so you can make informed decisions for your fasting practice.
Fasting and COVID-19 Infection
The COVID-19 pandemic has had immense impact worldwide. If you’re a frequent faster, it stands to reason you’d want to know what effects fasting might have on your immune health and COVID-19 infection risk. Put simply, fasting might be considered “training” for the immune system to keep active immune cells in tip top shape for inevitable exposures to pathogens including the COVID-19 virus.
Anything that supports and/or enhances overall health may help to reduce risks associated with COVID-19. Fasting could be a tool to do just that. Fasting decreases chronic disease and comorbidity risk by improving important markers of metabolic health. For an in-depth review of fasting physiology and COVID-19 Infection take a look at this review, which explores intermittent fasting as a priming tool for defense against COVID-19 in depth.
In addition to supporting metabolic health, fasting provides benefits to the immune system, specifically, by signaling autophagy. Autophagy contributes to cell surveillance processes that dismantle and recycle dysfunctional, lethal and mutant biomolecules, organelles, as well as invading pathogens to keep cells healthy. Several components of the immune system overlap those required for autophagy. In fact, viruses often block autophagy signaling pathways in order to ensure their own survival and replication; the COVID-19 virus (SARS-CoV-2) is no different. Routine autophagy stimulation through fasting has the opposite effect – it promotes immune system function and may help bolster your natural defenses against all infection, including COVID-19.
Much of the human research related to fasting effects on immune health specifically examines religious fasting practices such as Ramadan.These daily fasts usually span less than 24 hours (13-18 hours) over the course of 28-30 days. Ramadan fasting (sun-up to sun-down) for only four weeks has been shown to improve anticancer proteomic signature, DNA repair, and immune health markers. So all of the above should hold true for those of you with a fasting practice composed of shorter-term TRF fasts.
Prolonged fasting (48-120 hours) is a slightly different animal. Prolonged fasting can reverse immunosuppression and renew immune cells which benefits long-term immune health. However in the short term, it may result in a transient reduction in immune system strength, including decreased white blood cell count, until re-feed occurs. For this reason, we recommend limiting the duration of your fast, if you believe you may be at risk for contracting COVID-19.
Fasting and the COVID-19 Vaccine
The COVID-19 vaccines currently in use are so new that we do not yet have research data to make any direct claims about fasting alongside the COVID-19 vaccine in any of its various formulations. However, we do know a bit about how fasting impacts adaptive immunity which could play a part in the effectiveness of a vaccine.
Adaptive immunity – the part of our immune system that supports specialized identification and immune memory – is critical for vaccine efficacy. This portion of our immune system is diminished with age, a process known as “immunosenescence” which is especially pronounced for people over the age of 65.
Although our understanding is incomplete, researchers have seen some positive findings associated with fasting and a fast-mimicking diet in reversal of immunosenescence markers. It is useful to note that calorie intake is important for immune function. Chronic calorie restriction has been shown to reduce immune function, whereas short-term fasting followed by a dedicated re-feed promotes regeneration and immune system renewal. Previous research suggests calorically-adequate periodic fasting improves immune protection to infectious diseases or other challenges, and may support vaccine efficacy. We are on the lookout for any and all new research data related to fasting and COVID-19 vaccines.
Overall, a healthy lifestyle is a potent defense against disease. Fasting is just one of many health tools that you can use to prime your immune system against potential threats. Diet composition, physical activity, quality sleep, and meditation all play important roles as well.
If the sole focus of your fasting practice is immune strength, take care to ensure that you’re avoiding chronic caloric deprivation. In other words, make sure you’re eating enough during your eating window! And while fasting may serve as an immune system primer, prolonged fasting around the time of your vaccination may actually hinder your immune response. If you consider the COVID-19 vaccine to be an immune system exam, it’s probably not the best idea to do a prolonged 24+ hour “cram-session” (ie. fast) leading up to the injection. But if shorter, TRF fasting is already part of your health routine, there’s no reason to think you should change your “study” strategy. If you are feeling healthy, stick to what works for you!
About the Author: Rich LaFountain
Rich LaFountain is a science writer with a passion for exploring human health through lifestyle inputs, nutrition, and exercise. Rich completed his Bachelor of Science in Biology at The College at Brockport. He received his Master’s and Doctorate degrees in Kinesiology from The Ohio State University. He is fascinated by the manipulation of dietary patterns including fasting, macronutrient composition, and calorie restriction for targeted individualized outcomes in human health and performance.
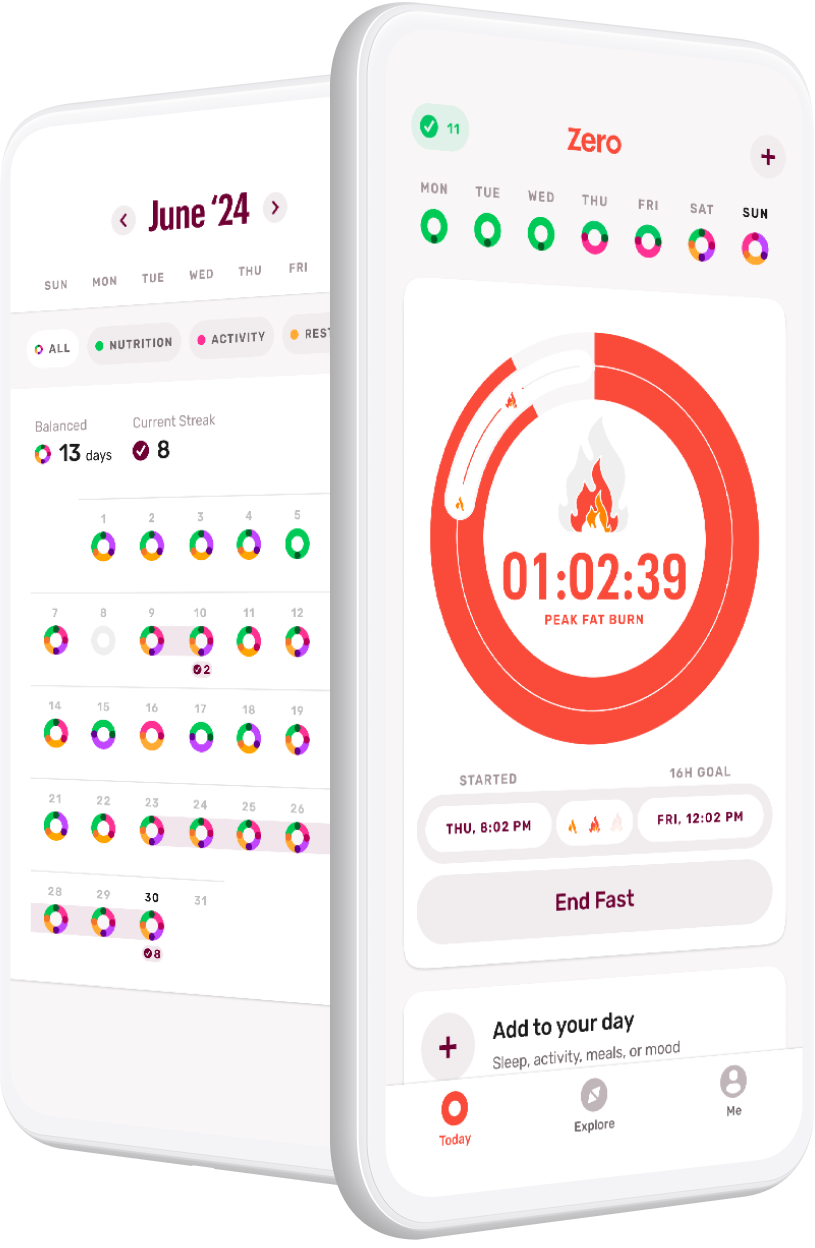
Download Zero on iOS and Android.
- Debunking 3 Myths Around Fasting and Thyroid Health - April 15, 2024
- Breaking Down Fast Breakers: How to Tell If Something Will Break Your Fast - March 4, 2024
- GLP-1s and Weight-Loss Medications vs. Lifestyle Interventions: What’s Right for You - February 5, 2024