Written and medically reviewed by Rich LaFountain, PhD
Everyone sleeps. It’s a basic need, like food, water, and movement, all of which are essential to life, health, and well-being. During sleep, your body focuses on recovery and repair, which requires a distinct metabolic state that is different from waking hours.
Unfortunately not everyone gets enough consistent, good-quality sleep. Impaired sleep, which dramatically increases chronic disease risk, impacts up to 40% of the general population — but there is something you can do about it. Just like you can refine your habits around other life essentials, you can set yourself up to get the quantity and quality of sleep you need to enhance both your healthspan and lifespan.
A Brief Sleep Primer
Sleep has a typical architecture, which is to say we all follow a pattern when we sleep. Throughout the night, we transition between two primary sleep states: non-rapid eye movement sleep (NREM) and rapid eye movement sleep (REM). Although these types of sleep are primarily classified based upon how your eyes move, they also differ in terms of electrical activity within your brain and your metabolic rate. During NREM sleep, your metabolic rate is lower, and specific neurochemicals like serotonin are elevated, whereas REM sleep is associated with spikes in acetylcholine. During REM sleep you are much more likely to dream, which is why REM sleep was once referred to as “dream sleep.”
Many research studies suggest that as you age, you sleep less and your sleep architecture shifts. Interestingly, in utero, mammals spend 50-80% of their day in REM sleep. That’s 12-19 hours a day! By adulthood, healthy sleep cycles last 80-120 minutes and are about 75% NREM and 25% REM sleep.
Good Sleep Is a Longevity Multiplier
We know that the best strategy to maximize our lifespan is to prevent or delay chronic disease. We also know that sleep is a necessity of life that is inextricably linked to metabolism and chronic disease. Therefore, prioritizing good sleep can set you up for a longer, healthier life, by protecting you from disease and positively influencing your metabolic well-being.
Here are five habits you can adopt to optimize sleep and improve longevity:
- Get enough sleep. According to the CDC, over one third of Amerians get less than 7 hours of sleep per night. Consistent shortened sleep duration contributes to molecular, immune, and neural changes that play a role in disease. Therefore, the first step in addressing sleep is to set up your routine so you get 7-9 hours of sleep nightly.
- Break sleep inertia early. For most people, sleep inertia, or grogginess immediately after waking, lasts 15-60 minutes. Whether or not you struggle with sleep inertia, adopting specific habits like viewing sunlight and prioritizing movement within the first hour of waking can help set your body’s circadian clock to get better sleep and reap sleep’s longevity benefits.
- If you nap, nap early. Naps certainly have a time and place: They can improve learning and memory consolidation through special brain waves called sleep spindles. However, naps too close to bedtime are bad for nighttime sleep. Researchers have found napping in the late afternoon or early evening can increase the time it takes to fall asleep after you turn out the lights by 30 minutes. Late-day naps can also double the duration of wake time at night, which interrupts sleep cycle phases and ultimately reduces sleep quality.
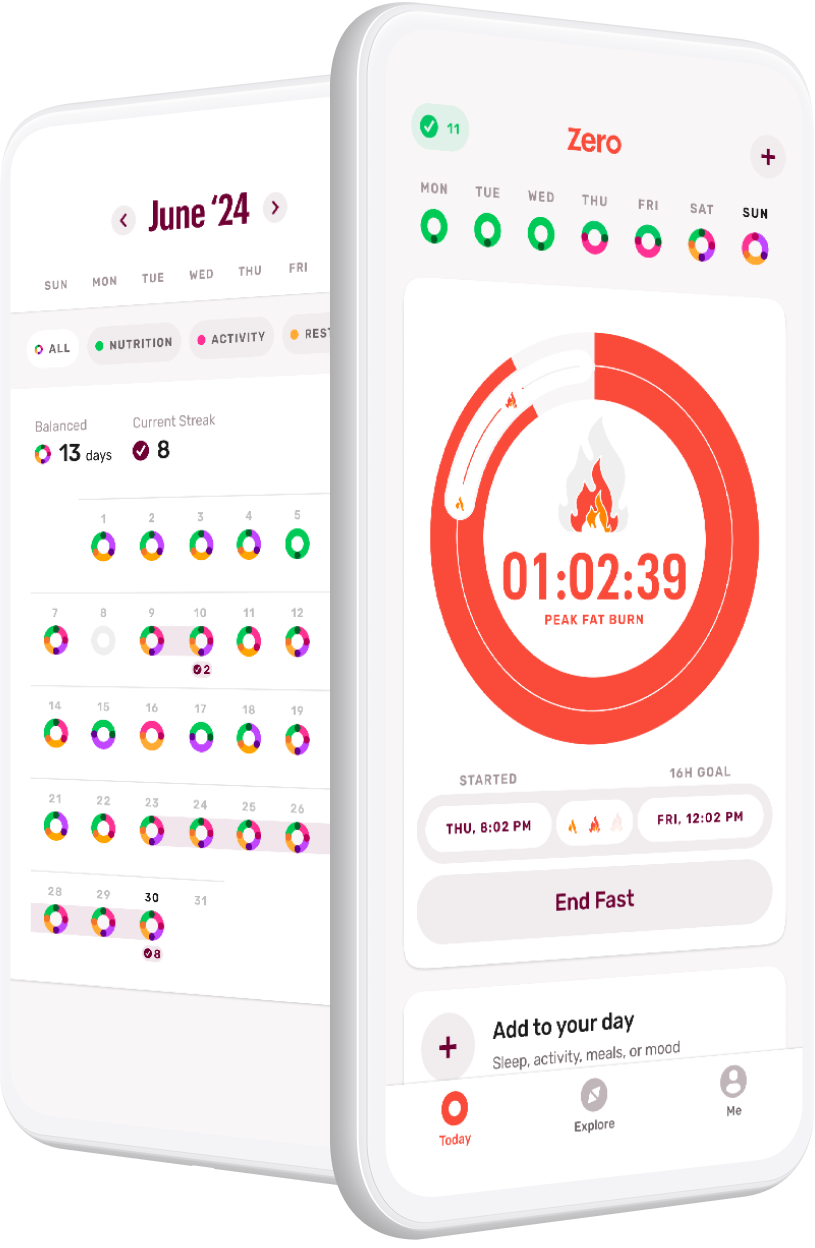
- Avoid consuming calories (including alcohol!) 2–4 hours before bed. Research shows meals, snacks, and alcohol disrupt sleep. Furthermore, eating meals and drinking alcohol after sunset, and especially close to bedtime, can sabotage your body’s opportunity to prioritize fat metabolism, which is a critical component of metabolic health. Thus, timing your meals to finish 2–4 hours before bed can help improve both your sleep and your metabolism.
- Maintain good sleep hygiene. Sleep hygiene refers to the behaviors and environmental factors that science shows are related to getting good-quality sleep. Examples include keeping a consistent sleep schedule, limiting light exposure, minimizing noise, and embracing mindfulness techniques, such as yoga nidra, prior to bedtime. Good sleep hygiene habits also include behaviors like avoiding caffeine up to 10 hours before bedtime and making sure any evening exercise happens at least 4 hours before bed.
Like it or not, we spend nearly a third of our lives sleeping. By ensuring that your sleep is sufficient and high-quality, you give yourself the opportunity to have more waking hours over a lifetime and to enjoy better health during every one of them.
References
Anafi, R. C., Kayser, M. S., & Raizen, D. M. (2019). Exploring phylogeny to find the function of sleep. Nature reviews. Neuroscience, 20(2), 109–116. https://doi.org/10.1038/s41583-018-0098-9
Luyster, F. S., Strollo, P. J., Zee, P. C., & Walsh, J. K. (2012). Sleep: a health imperative. Sleep, 35(6), 727-734. https://doi.org/10.5665/sleep.1846
Potter, G. D., Skene, D. J., Arendt, J., Cade, J. E., Grant, P. J., & Hardie, L. J. (2016). Circadian rhythm and sleep disruption: causes, metabolic consequences, and countermeasures. Endocrine reviews, 37(6), 584-608. https://doi.org/10.1210/er.2016-1083
Ji, X., Grandner, M. A., & Liu, J. (2017). The relationship between micronutrient status and sleep patterns: a systematic review. Public health nutrition, 20(4), 687–701. https://doi.org/10.1017/S1368980016002603
McCarley R. W. (2007). Neurobiology of REM and NREM sleep. Sleep medicine, 8(4), 302–330. https://doi.org/10.1016/j.sleep.2007.03.005
Ursin, R. (2002). Serotonin and sleep. Sleep medicine reviews, 6(1), 55-67. https://doi.org/10.1053/smrv.2001.0174
McCarley R. W. (2007). Neurobiology of REM and NREM sleep. Sleep medicine, 8(4), 302–330. https://doi.org/10.1016/j.sleep.2007.03.005
Crick, F., & Mitchison, G. (1983). The function of dream sleep. Nature, 304(5922), 111–114. https://doi.org/10.1038/304111a0
Ohayon, M. M., Carskadon, M. A., Guilleminault, C., & Vitiello, M. V. (2004). Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep, 27(7), 1255-1273. https://doi.org/10.1093/sleep/27.7.1255
Pignolo R. J. (2019). Exceptional Human Longevity. Mayo Clinic proceedings, 94(1), 110–124. https://doi.org/10.1016/j.mayocp.2018.10.005
Kim, D., Hoyos, C. M., Mokhlesi, B., Pamidi, S., & Jun, J. C. (2020). Editorial: Metabolic Health in Normal and Abnormal Sleep. Frontiers in endocrinology, 11, 131. https://doi.org/10.3389/fendo.2020.00131
Centers for Disease Control and Prevention (CDC) (2011). Effect of short sleep duration on daily activities–United States, 2005-2008. MMWR. Morbidity and mortality weekly report, 60(8), 239–242.
Watson, N. F. et al. (2015). Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep, 38(6), 843–844. https://doi.org/10.5665/sleep.4716
Hilditch, C. J., Dorrian, J., & Banks, S. (2016). Time to wake up: reactive countermeasures to sleep inertia. Industrial health, 54(6), 528–541. https://doi.org/10.2486/indhealth.2015-0236
Kaplan, K. A., Talavera, D. C., & Harvey, A. G. (2018). Rise and shine: A treatment experiment testing a morning routine to decrease subjective sleep inertia in insomnia and bipolar disorder. Behaviour research and therapy, 111, 106–112. https://doi.org/10.1016/j.brat.2018.10.009
McGlinchey, E. L., Gershon, A., Eidelman, P., Kaplan, K. A., & Harvey, A. G. (2014). Physical activity and sleep: Day-to-day associations among individuals with and without Bipolar Disorder. Mental health and physical activity, 7(3), 183–190. https://doi.org/10.1016/j.mhpa.2014.05.003
Richardson, G., & Tate, B. (2000). Hormonal and pharmacological manipulation of the circadian clock: recent developments and future strategies. Sleep, 23 Suppl 3, S77–S85.
Clawson, B. C., Durkin, J., & Aton, S. J. (2016). Form and Function of Sleep Spindles across the Lifespan. Neural plasticity, 2016, 6936381. https://doi.org/10.1155/2016/6936381
Werth, E., Dijk, D. J., Achermann, P., & Borbély, A. A. (1996). Dynamics of the sleep EEG after an early evening nap: experimental data and simulations. The American journal of physiology, 271(3 Pt 2), R501–R510. https://doi.org/10.1152/ajpregu.1996.271.3.R501
Werth, E., Dijk, D. J., Achermann, P., & Borbély, A. A. (1996). Dynamics of the sleep EEG after an early evening nap: experimental data and simulations. The American journal of physiology, 271(3 Pt 2), R501–R510. https://doi.org/10.1152/ajpregu.1996.271.3.R501
Crispim, C. A., Zimberg, I. Z., dos Reis, B. G., Diniz, R. M., Tufik, S., & de Mello, M. T. (2011). Relationship between food intake and sleep pattern in healthy individuals. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 7(6), 659–664. https://doi.org/10.5664/jcsm.1476
Thakkar, M. M., et al. (2015). Alcohol disrupts sleep homeostasis. Alcohol (Fayetteville, N.Y.), 49(4), 299–310. https://doi.org/10.1016/j.alcohol.2014.07.019
Nakajima K. (2018). Unhealthy eating habits around sleep and sleep duration: To eat or fast?. World journal of diabetes, 9(11), 190–194. https://doi.org/10.4239/wjd.v9.i11.190
Jiang, P., & Turek, F. W. (2017). Timing of meals: when is as critical as what and how much. American journal of physiology. Endocrinology and metabolism, 312(5), E369–E380. https://doi.org/10.1152/ajpendo.00295.2016
Riedel, B. W. (2000). Sleep hygiene. In K. L Lichstein & C. M Morin (Eds.), Treatment of late-life insomnia (pp. 125–146). Sage Publications, Inc.
Gellis, L. A., & Lichstein, K. L. (2009). Sleep hygiene practices of good and poor sleepers in the United States: an internet-based study. Behavior therapy, 40(1), 1–9. https://doi.org/10.1016/j.beth.2008.02.001
Datta, K., et al. (2021). Yoga nidra practice shows improvement in sleep in patients with chronic insomnia: A randomized controlled trial. The National medical journal of India, 34(3), 143–150. https://doi.org/10.25259/NMJI_63_19
- Debunking 3 Myths Around Fasting and Thyroid Health - April 15, 2024
- Breaking Down Fast Breakers: How to Tell If Something Will Break Your Fast - March 4, 2024
- GLP-1s and Weight-Loss Medications vs. Lifestyle Interventions: What’s Right for You - February 5, 2024