Written and medically reviewed by Katya Meyers, RD
Females bodies are complex, intricate, and ever-changing feats of evolution. And there may be no stage of life when this is more apparent than during the gradual transition from the reproductive to post-reproductive years known as menopause.
Despite what you may have heard, menopause isn’t all bad. In fact, in Eastern medicine, menopause is known as a “second spring” — a prelude to the next chapter of good things to come. That’s not to say that the menopausal transition is seamless; natural hormonal fluctuations during perimenopause and menopause can lead to physiological and emotional changes that aren’t always pleasant. An increase in body fat, as well as changes in body-fat distribution, hot flashes, night sweats, a decline in energy, changes in mood, and sleep disturbances are just some of the very real effects of a changing hormone milieu for aging females. However, with the right outlook and healthy habits — anchored, of course, by intermittent fasting — this new season of life is one you can embrace.
An Introduction to Menopause, Perimenopause, and Postmenopause
Perimenopause marks the transitional phase from the reproductive years to menopause. It begins with menstrual irregularities, usually beginning in a female’s 40s (although it can start earlier or later) and ends one year after the final menstrual period. As ovarian function declines, estrogen, progesterone, follicle-stimulating hormone, and other sex-hormone levels can fluctuate wildly. Many women will experience resulting mood swings, hot flashes, sleep disruptions, and changes in sexual function during this phase. However, both the duration and severity of everyone’s symptoms vary. Certain medications, various forms of birth control, and the addition of hormone-replacement therapy are just a few factors that can influence how females experience this transition.
Menopause is defined as the cessation of menstruation for 12 consecutive months. Following the final menstrual period — sometimes quickly, sometimes not — the rapid fluctuations in hormone levels that began in perimenopause slow, and estrogen and progesterone levels drop drastically. It is this lower level of estrogen that is responsible for many of the symptoms associated with menopause. Androgens (male sex hormones) such as DHEA and testosterone also shift, with the relative ratio of testosterone to estrogen increasing during menopause (although the actual amount of free testosterone present may decline). Research shows that this “new normal” balance of hormones often promotes weight gain and a pattern of central adiposity (abdominal fat), which most females would likely prefer to do without. However, everyone’s experience is different, and lifestyle modifications — including intermittent fasting — can help to mediate these changes.
“Navigating this journey with thousands of women, it’s inspiring to see how much we can impact this process with a bit of knowledge and a plan of action. It is possible to avoid the unhealthy weight gain known as visceral fat. Fasting and other lifestyle behaviors around nutrition, movement, sleep, and connecting with others can really make a difference in how you feel moving through and on the other side of the menopause transition,” says Dr. Naomi Parrella, Zero’s Chief Medical Officer.
Although menopause marks the end of one phase, it also marks the beginning of another! The average age of menopause is 51, while the U.S. life expectancy for females is just over 79, leaving plenty of postmenopausal years to enjoy personal and professional growth and development. During postmenopause, hormone levels stabilize, and while occasionally some symptoms of menopause may persist, postmenopausal women typically enjoy a reduction in symptoms and a renewed zest for life. Research also reveals that, on average, women are happier during this postmenopausal phase, with life satisfaction scores increasing as women move beyond 65 years of age. This is no surprise to Dr. Parrella, who works with men and women of all ages.
“The postmenopausal years mark the time women can truly blossom and turn their attention to pursuing the most important things to them,” says Dr. Parrella. “This is the stage of life when you get more choice about how you spend your time, what and when you eat, and what new habits and lifestyle behaviors you want to adopt as you enter this new chapter.”
Fasting Considerations for Each Stage of Menopause
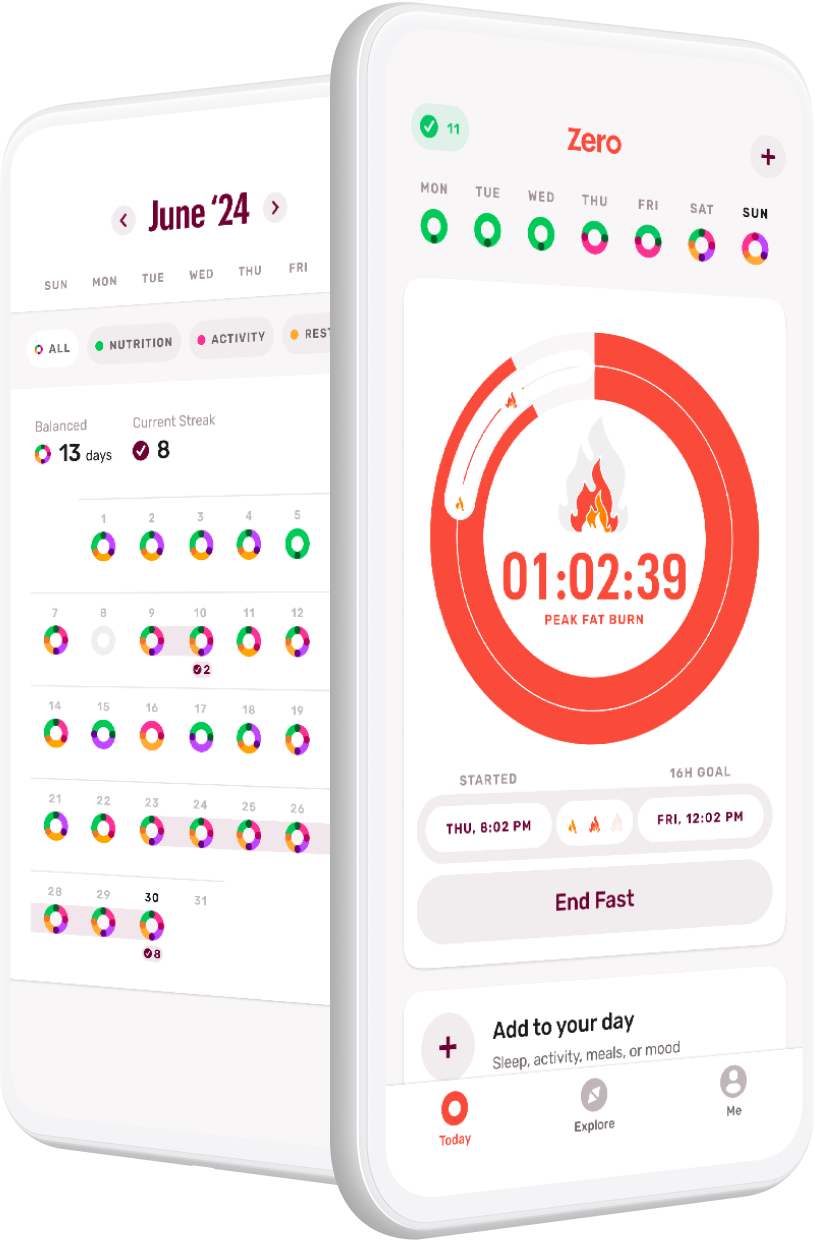
Fasting offers several benefits that may help you dance gracefully across the stages of menopause, rather than white-knuckling your way through. Lengthening your fasting window to 12–18 hours each day has been shown to increase epinephrine (which boosts metabolism) and growth hormone (which promotes protein synthesis necessary for lean mass) as well as decrease insulin (which turns on fat burning), all of which are helpful for maintaining a healthy weight throughout the menopause transition. Moreover, thanks to fasting’s ability to help regulate hormone levels, females who adopt an intermittent-fasting practice may find relief from many of the symptoms of menopause, such as hot flashes, mood swings, and disrupted sleep.
Each stage of menopause comes with its own unique set of considerations pertaining to fasting. Weight and heart health are the chief concerns during perimenopause, while bone health and lean body mass come to the forefront during menopause and postmenopause.
Perimenopause
Definition: The months and years during which menstrual irregularities begin as your reproductive system starts to shut down.
Because it’s effective at promoting weight loss and fat loss, intermittent fasting can also mitigate some of the metabolic concerns of perimenopause, like insulin resistance, weight gain, and increased abdominal fat. Research suggests that intermittent fasting may offer promising solutions to the challenges of perimenopause by minimizing weight gain, maintaining insulin sensitivity, and reducing inflammation. Studies show that weight management and maintaining insulin sensitivity are particularly pertinent during this transitional phase due to the increased risk of cardiovascular disease that accompanies perimenopause. Additionally, insulin resistance, weight gain, and increased abdominal fat can also be risk factors for increased menopausal symptoms. Therefore, by using intermittent fasting to overcome them, females can lessen their chances of suffering severe hot flashes, disrupted sleep, and other undesirable symptoms.
Menopause
Definition: The 12 months after your final menstrual period.
The years of fluctuating hormones around and after menopause are the time of greatest muscle and bone loss due to lower levels of estrogen and progesterone. Additionally, during this time, that lack of estrogen combined with higher insulin levels can lead to a progressively enlarging waistline. Disordered sleep can add to the weight gain, and the more weight you gain, the further you aggravate insulin resistance, which leads to more cravings, worse blood-sugar control, and increased cardiovascular risk factors.
“The goal is to counter this spiral with the combined power of fasting, nutrition, and necessary muscle-strengthening activities to stimulate bone and muscle maintenance,” says Dr. Parrella. Therefore, during menopause and beyond, put extra emphasis on meeting your nutrient needs, such as calcium, vitamin D, and protein during your eating window, and engage in consistent load-bearing exercise (walking, jogging, dancing, lifting weights) in order to maintain strong muscles and bones.
Postmenopause
Definition: The months and years following menopause, during which your reproductive functions have ceased.
As females enter this later stage of life, the preservation of lean body mass becomes paramount. While research shows that intermittent fasting can be more protective of lean body mass during weight loss than regular caloric restriction (a.k.a. most diets), it’s essential to ensure that your eating window is long enough and that you’re eating the best foods to satisfy your protein goals in the postmenopause years.
In addition, combining intermittent fasting with additional healthy habits, like exercise, can help you double down on the benefits of fasting during this stage of life. A recent study of postmenopausal females with obesity showed that pairing fasting with physical-cognitive exercise (i.e., movement that challenges both the body and the brain) can improve memory and executive function as well as metabolic biomarkers, such as insulin levels. Promoting brain health earlier in life can lower your risk of developing cognitive impairment later in life.
What Other Healthy Habits Should You Include in Your Menopausal Journey?
Establish a Good Nighttime Routine
Many women experience sleep disturbances as they enter perimenopause. While hot flashes can disrupt your shuteye, so too can poor metabolic health. One study found women with metabolic syndrome averaged 15 minutes less sleep, as well as poorer quality sleep, than those with better metabolic health. In fact, this is likely a bidirectional relationship, as getting the right amount of quality sleep each night can improve satiety and make weight loss easier.
To work towards improving your metabolic health — and perhaps also lessen your perimenopause and menopause symptoms — establish a good nighttime routine for your best chance of getting a great night of sleep. This includes keeping sleep and wake times consistent, turning off all electronics at least an hour before bed, and starting your Timer 2–3 hours before hitting the pillow.
Start (or Continue!) Strength Training
The idea that your metabolism steadily grinds to a near halt in middle age and beyond is a myth. The truth is that there is very little inherent age-related decline in your resting metabolic rate (RMR), i.e., the amount of energy your body burns at rest. However, RMR is strongly correlated to lean body mass, which typically decreases as you age due to both changes in hormones and — often, but not always — a decline in daily movement during menopause and beyond.
The solution is to include regular strength training in your repertoire of daily activities! Muscle doesn’t just help your body move better, it also burns more calories while you’re at rest and improves insulin sensitivity — both good things for losing weight, burning fat, and maintaining metabolic health. Plus, strength training benefits more than just muscle. “Weight-bearing exercise is beneficial for maintaining bone strength, too,” says Dr. Parrella. “And of course, exercise of any kind is shown to boost mood and feelings of self-efficacy.”
Interrupt Sedentary Activity
Interrupting sedentary activity is not just another way of saying “exercise more.” Rather, it’s about replacing prolonged sitting with more standing, walking, and other types of general movement throughout your day. Research shows that the vast majority of our energy expenditure doesn’t come from workouts (except in the edge cases of some highly competitive athletes), but from the more mundane daily activities — things like walking to the office copy machine, putting away laundry, or unloading the car.
In addition to burning more calories, increasing your amount of low-intensity activity can help you realize the cardiometabolic benefits of the exercise you are already doing. In an Australian study of women who already met or surpassed the recommended 150 minutes of moderate activity each week, those who spent less time viewing TV had less obesity, smaller waist circumference, and better fasting glucose levels. Moral of the story? Even if you’re someone who already exercises vigorously most days of the week, you’ll want to try and move more throughout the day to best match your energy needs and improve your overall metabolic health.
Cook More Meals at Home
No matter what phase of life you are in, eating more whole foods is an excellent addition to your health routine — and cooking at home is a simple way to achieve that. Research shows that home-cooked meals are lower in calories and higher in fruit and vegetable content than prepackaged meals or meals eaten out. Therefore, it follows that those who cook at home at least five times per week are 28% less likely to be overweight or obese. You also may be less inclined to order a drink (or three) to “be social,” and drinking less alcohol at this life stage is a good idea because alcohol can more easily lead to belly fat, according to Dr. Parrella.
Reduce Stress and Cultivate a Positive Self-Image
One study found that menopausal women with the most psychological distress and negative body image were more likely to engage in emotional eating to combat distress. Unfortunately, this tends to create a downward spiral, as emotional eating is tightly correlated with weight gain and difficulty self-regulating during weight-loss attempts. “The spiraling effect comes from chronically elevated cortisol, which leads to increased blood sugar, which leads to increased insulin, which turns off fat burning. When fat burning turns off, the body perceives a lack of fuel. Its response is to generate cravings that cause us to overeat, often poor-quality foods, which leads to gaining visceral or abdominal fat. This further worsens insulin resistance and keeps fat burning turned off, leading to further cravings, fat storage, and a growing waistline,” says Dr. Parrella. In other words, stressing about the number on the scale is likely to backfire and take you even further from your goals.
To generate a more positive self-image, focusing less on how your body looks and more on all the amazing ways it performs is a good place to start. Other ways to escape the cycle of emotional eating include engaging in physical activity, mindful eating, and stress-reducing activities like breathwork, meditation, and yoga.
Conclusion: Menopause Is NOT a Problem
Menopause is often described as the end of a female’s reproductive years. But menopause does not simply mark an end; it also marks a beginning. The reality is, menopause and its various phases are a healthy part of what female bodies are naturally designed to do. Armed with the right knowledge and support, it is possible to navigate this natural transition with confidence, health, and vitality. Including intermittent fasting in your daily routine can help to ameliorate many of the concerns you may have about menopause, as can adopting healthy habits such as a good nighttime routine, consistent strength training, more daily movement and home-cooked meals, and a regular stress-reduction practice.
- The Fasting Guide to Menopause, Perimenopause, and Postmenopause - April 8, 2024
- Try This Instead of That: How to Bookend Your Fasts - March 25, 2024
- 60 Names for Sugar: The Myths, The Facts, and What You Should Know - February 12, 2024