Written and medically reviewed by Naomi Parrella, MD
My passion has always been to help people feel good and thrive! Therefore, throughout my career, I’ve focused on supporting people’s health, particularly through connecting behavior and thought patterns with how the body works. As it turns out, this often leads to success in many areas of life and especially in successful, long-term weight management.
Weight Is Tied to Metabolic Health
In the United States, our life expectancy is 77 years, but in countries like Switzerland, Australia, and Japan, life expectancy is 83 to 84 years. What is the difference? Roughly three out of every four American adults are either overweight or obese. This is relevant because overweight and obesity are often associated with poor metabolic health. This, in turn, increases disease risks and complications and shortens healthy life expectancy.
What Is Metabolic Health?
Metabolic health is about how well your body manages and uses fuel. To be alive, you need three things: (1) fuel, which is primarily glucose or fat; (2) the ability to convert fuel to energy; and (3) the ability to use that energy. Therefore, metabolic health is the ability to convert glucose or fat into energy, which your body can then use.
If you are metabolically healthy, your body is able to seamlessly switch between burning glucose and fat depending upon your energy needs and energy availability so you always have sufficient fuel. This “switching” is called metabolic flexibility. Research supports that if you’re metabolically healthy, meaning you have good metabolic flexibility, the risk for chronic health problems like diabetes, high blood pressure, overweight and obesity, cancers, and dementia may be lower.
Unfortunately, over 93% of Americans are not metabolically healthy; they have some form of metabolic dysfunction which can lead to high blood pressure, heart disease and strokes, poor sleep and sleep apnea, prediabetes, diabetes, infertility, increased risk of multiple cancers, dementia and mental-health concerns like depression and anxiety, and painful conditions like arthritis and immobility. These conditions are linked by the fact that metabolic dysfunction leads to inflammation and low energy, and it impairs the immune system. As a result, the body is compromised so it takes longer to heal — even from typically shorter-term ailments like wounds or an infection.
How Is Metabolic Health Measured?
In the medical profession, metabolic health is most commonly assessed by measuring blood sugar, waist circumference, blood pressure, HDL cholesterol, and triglycerides. If all of these numbers are within a favorable range, they likely represent a body that is effectively managing fuel and energy resources.
So, why have I focused on weight?
Unintentionally gaining extra weight, especially around the waistline, is one of the first signs of metabolic dysfunction. There are a lot of people affected by excess weight, and regardless of where they are starting, they don’t want the unnecessary risk of further health problems associated with metabolic dysfunction. They may aspire to feel better and get healthier — they just need the right support. So I focus on weight because the science shows that maintaining a healthy weight is associated with both healthspan and lifespan.
How My Approach to Weight Loss Has Changed
Early on, I used to teach people about calories in, calories out: “Just eat less and exercise more, and the weight will miraculously drop.” Over time, however, I found that people’s weight-loss success rates always slid back to 0%. Often, they would lose some weight, maybe 5–10 pounds, but then rebound back up. I asked my colleagues: “What am I missing?” They replied that the participants were likely just not reporting correctly, that they were actually eating more and exercising less than they claimed. However, I was teaching an exercise class to some of these people. I saw them exercising in my classes, so I knew their estimates could not be that far off.
Upon further reflection, I realized that the only common part of each person’s story was the “calories in, calories out” advice I was giving them. I needed new advice. When I dove into the literature and weight-loss stories from around the world, I discovered people who had achieved long-term weight-loss success — plus improved energy levels and greater feelings of control — without feeling hungry. Clearly, there was another way. It was time to start really collaborating with my patients to try new approaches.
One of my patients with type-2 diabetes who was treated with insulin at the time decided she wanted to try fasting. Her endocrinologist was not in favor, but her recent labs had shown her blood sugars were going in the wrong direction, so we decided to trial this new eating pattern for three months and see what happened. We’d decide based on data.
The first week was tough for my patient. She reported that it felt like a withdrawal period — headaches, fatigue, and malaise. But by week two, she noticed that her pants were fitting better and she felt a bit better overall. Her asthma seemed to have calmed down, and she didn’t notice as much joint pain. I was amazed. Could it be a placebo effect?
Over time, she lost weight, started moving more, was able to stop insulin, took fewer medications, slept better, and became very cheerful. The cravings that had plagued her were under control. It turned out that her issue wasn’t a lack of discipline, as she had believed. Her eating pattern had taken over her hormone signaling in a way that did not serve her. In the end, her three-month labs were so good that her endocrinologist called me to ask more about what she was doing. He wanted to recommend her protocol to other patients.
What Was Getting in the Way?
What this patient and so many of my other patients have achieved is renewed metabolic flexibility, i.e., the ability to switch between glucose and fat for your energy needs. Metabolic flexibility is impacted by fasting, nutrition, movement, and stress, and it’s when you lose metabolic flexibility that your body “panics” and sends out hunger alerts because it doesn’t have access to the fuel it needs. Unfortunately, many people have lifestyles and habits that lock them into a glucose-burning pattern that inhibits their metabolic flexibility and ability to burn the fuel that is virtually always available, fat.
The obstacles to healthy living — and consequent metabolic health — are many. For example, on average, most people eat calories for nearly 15 hours or more each day, which means that their body rarely or never moves into a fat-burning state. Additionally, physical activity rates have declined over 30% since the 1960s, average sleep duration is roughly 6.8 hours (down from 9 hours a century ago), and chronic stress is more prevalent than ever. (According to the American Institute of Stress, over 75% of all doctor visits are now stress-related!) All of these declining health habits can lead to metabolic dysfunction.
As an example, many people often report getting hungry roughly 1–4 hours after a meal or snack. As the body has burned off or stored the fuel from the meal or snack, it needs to switch to burning the stored fuels on the body — glycogen or fat. With metabolic flexibility, switching to glycogen and fat burning is easy and natural, and the wave of hunger passes. Without that flexibility, hunger increases, cravings become the norm, and the drive to survive kicks in, so it feels impossible to be in control until finding something to eat or drink.
This can partially explain late-night munchies. Late-night snacking is so common because your body is almost finished burning the fuel you consumed at dinner. If you are metabolically flexible, that late night9–11 p.m. craving is diminished or may go entirely unnoticed as your body seamlessly shifts to burning stored energy (like glycogen or fat) without signaling a need for more food. The good news is that even if you’re someone experiencing these cravings, you can train your body to become more metabolically flexible.
Using the #1 Tool for Building Metabolic Health
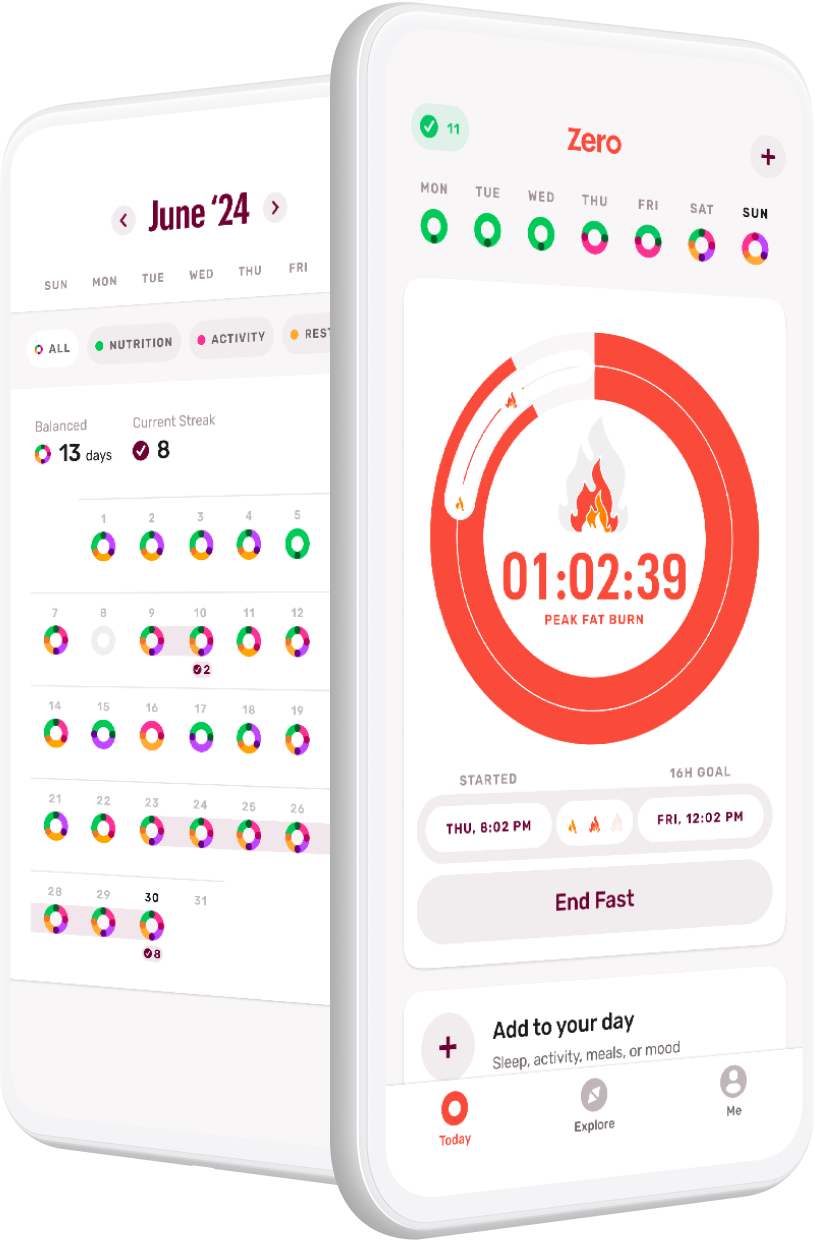
Once my patients understand their metabolic health and can recognize which lifestyle choices are interfering with their metabolic flexibility, it’s time for an intervention. Years ago, a wildly successful patient introduced me to Zero. Since then, one of my favorite tools to help individuals systematically overcome some of these obstacles to health has been Zero.
Zero makes it easy to start building the foundational habit of intermittent fasting, which reintroduces the body to its own natural fat-burning capacity. With this habit locked in, the app then helps individuals layer on additional habits — even really simple ones, like getting enough sleep and moving every day — that together form a balanced approach to health.
Ultimately, Zero is a great tool for building metabolic health through habit formation because it adds elements of accountability, fun, and learning to what otherwise can often feel like prescriptive “interferences” in what was once your daily routine. I continue to guide my patients to use Zero today, and they continue to see lasting results.
Conclusion: Maintaining a Healthy Weight Is Associated with Both Healthspan and Lifespan
I love that I have the opportunity to work with patients directly, and partnering with Zero will enable more people to learn and deploy proven strategies as they experience lasting weight-loss success and improve their metabolic health. If you’re interested in learning more about how Zero can help you, come join us for the next Zero Live!
- Q&A with Dr. P: Weight Management Tips & Tricks - June 6, 2024
- Q&A with Dr. P: Weight-Loss Plateaus, Fasting Metabolism, and More - April 22, 2024
- Bridging the Gap: Eastern and Western Medicine in Modern Times - March 11, 2024