Written and medically reviewed by Naomi Parrella, MD
Eastern and Western medicine can be easily misunderstood. There may be staunch advocates of Eastern medicine who point out that their approach to health is more holistic, while Western medicine proponents emphasize the fact that their treatments are backed by science. However, both forms of medicine have the same goal: promoting healing and health. Therefore, rather than thinking that you can only pick one way or the other, it is entirely possible to choose an approach that integrates the best of both to achieve optimal outcomes.
What’s the Difference Between Eastern and Western Medicine?
Eastern medicine is a system that has been used for thousands of years to prevent, diagnose, and treat disease. In general, Eastern medicine entails looking at the “whole picture” of a person’s spiritual, emotional, mental, and physical health to identify what’s causing problems and then providing treatment that removes the barriers to healing and recovery. There is a trust that by treating the cause, the body will heal itself. Eastern medicine encompasses specially trained practitioners who apply acupuncture, diet, herbal therapy, meditation, physical exercise, and massage to heal patients. Proponents of Eastern medicine cite prevention, personal ownership, and patient agency as key advantages of this system of medicine.
Western medicine is a system in which medical doctors and other healthcare professionals such as nurses, pharmacists, and therapists treat symptoms and diseases using drugs, radiation, or surgery. Western medicine also goes by the names conventional medicine, allopathic medicine, biomedicine, or orthodox medicine. No matter its name, Western medicine relies on scientific research, precision, and technological advancement, all of which are anchored by a patient’s diagnosis. It is particularly effective at treating acute problems that require an immediate response — a broken leg, bacterial infection, or collapsed lung can be effectively treated with quick Western-medicine interventions. And thanks to the advent of antibiotics and an improved understanding of infectious pathogens and sterile techniques, life expectancy has more than doubled since the 1800s.
Based on these definitions, it may appear that Eastern and Western medicine are polar opposites. However, there is striking overlap between the two.
Exploring Eastern Medicine
A Brief History of Eastern Medicine
Eastern medicine, which originated with ancient civilizations located in China, India, and Egypt, predates Western medicine by hundreds, if not thousands, of years. For instance, Ayurveda, the traditional healing system of India, dates back over 5,000 years. Eastern medicine continues to evolve, and it remains a vibrant and integral part of healthcare systems around the globe today. Ongoing scientific exploration of Eastern-medicine practices have validated some traditional techniques, including acupuncture, diet, exercise, and intermittent fasting, which are now supported by robust and growing research literature that informs us about the healing properties of ancient medical practices.
What Are Some Common Practices in Eastern Medicine?
Originating from China, acupuncture is a quintessential Eastern-medicine practice that involves inserting thin needles into specific points on the body to restore the flow of energy and alleviate symptoms. In addition to acupuncture, other common practices include herbal medicine, cupping therapy, tai chi, and qigong (exercise).
Ayurveda is an ancient healing system from India that utilizes herbal remedies, dietary guidelines, yoga, and meditation to promote health and balance. Yoga, which also originated in India, is another very common holistic discipline that combines physical postures, breathing exercises, and meditation to enhance overall well-being and promote harmony within the body and mind. It’s worth noting that many common Eastern-medicine practices are part of a healthy lifestyle in which nutrition, exercise, sleep, and stress are all managed through regular behaviors and habit structure.
What Are the Potential Benefits and Challenges of Eastern Medicine?
Eastern medicine offers several advantages, including its holistic approach to health, which recognizes the interconnectedness of the body, mind, and spirit. By addressing underlying imbalances and promoting harmony within the body’s systems, Eastern medicine aims to not only alleviate symptoms but also enhance general well-being. Additionally, many practices within Eastern medicine, such as acupuncture, herbal medicine, and yoga, have been used for centuries and have accumulated a wealth of empirical evidence supporting their efficacy in treating various health conditions. Furthermore, Eastern medicine often emphasizes accessible remedies and lifestyle modifications, which can empower individuals to take an active role in their own health and promote preventive care.
That said, Eastern medicine faces several challenges, particularly in the integration with Western medical systems. Variability in training and regulation among Eastern medicine practitioners can lead to inconsistent quality of care or even safety concerns. Additionally, some aspects of Eastern medicine, such as acupuncture and herbal remedies, may lack standardized protocols and rigorous scientific validation, making it difficult for Western healthcare providers to fully endorse Eastern or “alternative” medicine. Despite these challenges, efforts to bridge the gap between Eastern and Western medicine through scientific investigation are underway, with increasing recognition of the potential benefits of combining the strengths of both systems to provide comprehensive and personalized care to patients.
Exploring Western Medicine
A Brief History of Western Medicine
Western medicine has roots in ancient Greece and Rome, where there was a decidedly rational and scientific approach to medicine. The development of the scientific method in the 17th century laid the foundation for modern medicine. The 19th and 20th centuries witnessed rapid progress in medical science, including the discovery of microbes (germ theory), the development of vaccines and antibiotics, and the advent of modern surgical techniques and diagnostic technologies. Today, Western medicine is characterized by its evidence-based approach, specialization, and reliance on pharmaceutical drugs, surgery, and advanced technology to diagnose, treat, and occasionally prevent illness.
What Are Some Common Practices in Western Medicine?
Common practices in Western medicine encompass a broad range of diagnostic, therapeutic, and preventive interventions aimed at addressing diagnoses based on signs and symptoms linked with health, injury, and disease. Western medicine tends to view the body through the lenses of physiology and pathophysiology of disease; therefore, clinical evaluations involving medical-history reviews and physical examinations, pharmaceutical interventions to manage symptoms and treat diseases, surgical procedures, and diagnostic technologies such as imaging studies and laboratory tests are all used to attempt to accurately diagnose and treat patients.
Western medicine also employs preventive measures, such as vaccinations and screenings, to identify and mitigate health risks. Vaccinations, which are not relied on in Eastern medicine, have proven effective in dramatically reducing or nearly eliminating select diseases from public circulation. In sum, Western medicine has revolutionized the way that humans are able to leverage science in order to treat disease and reduce risk to the physical body.
What Are the Potential Benefits and Challenges of Western Medicine?
The primary benefits of Western medicine include its evidence-based approach, which emphasizes rigorous scientific research and clinical trials to ensure the safety and efficacy of treatments. This focus on evidence allows for the development of standardized protocols and guidelines that inform clinical practice and aim to improve patient-outcome consistency. Additionally, Western medicine offers advanced diagnostic technologies and specialized medical expertise, enabling more specific diagnoses and precision treatments for a wide range of health conditions. Moreover, Western medicine places a strong emphasis on vaccinations, screenings, and lifestyle modifications for preventive care, which help reduce the incidence of diseases and are intended to improve overall public health.
Nevertheless, Western medicine faces several challenges. One imminent challenge is the rising cost of healthcare, driven by factors such as the high cost of pharmaceuticals, advanced medical technologies, and exorbitant administrative expenses, which can easily strain family budgets. The high cost of Western medicine contributes to disparities in access to care or forgoing care altogether due to financial burden.
Additionally, Western medicine’s focus on treating specific symptoms and diseases may sometimes overlook the interconnected nature of health and fail to address underlying root causes of illness. Relatedly, Western medicine’s specialization and compartmentalization of healthcare can sometimes result in fragmented care and communication gaps between healthcare providers, leading to suboptimal outcomes for patients. Finally, there are concerns about overreliance on pharmaceutical drugs and the potential for adverse effects and waning efficacy. Addressing these challenges requires ongoing efforts to improve healthcare affordability, promote holistic approaches to health, and build interdisciplinary collaboration within the healthcare system.
How Can Eastern and Western Medicine Coexist?
Eastern and Western medicine can and should be paired for ideal health outcomes by adopting an integrative healthcare approach that leverages the strengths of both systems.
First, the two approaches to health should not be seen as mutually exclusive. Most pharmaceutical interventions in Western medicine, for instance, are plant-based and would therefore qualify as an Eastern medicine herbal therapy. Similarly, many techniques and even entire fields of Western medicine, such as physical therapy, are rooted in Eastern medicine approaches.
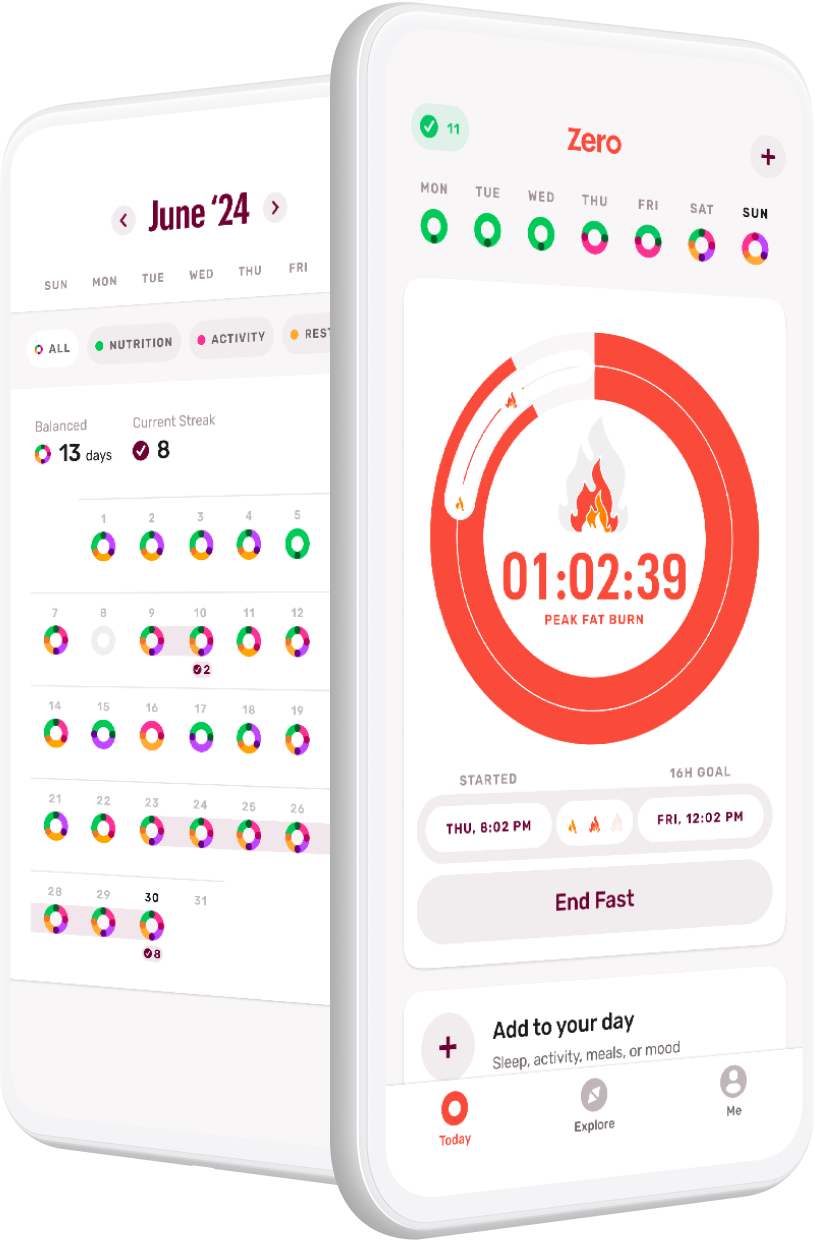
Perhaps most notably, if you love Zero and practice intermittent fasting for your health, you are applying an ancient Eastern medicine practice that, over the last century, has amassed significant Western-medicine research evidence — first as an effective therapeutic for patients with diabetes in the late 19th century, and then as a treatment for epilepsy in the early 20th century. Contemporary research focuses on fasting as an evidence-based strategy for preventing and treating a whole range of conditions and diseases while promoting health and longevity.
Next, healthcare providers should collaborate to develop personalized treatment plans that address the root causes of illness while managing symptoms effectively. In Western medicine, practitioners are often quick to match labels like diabetes, overweight, or obesity to symptoms, and move straight to the fastest-acting treatment that will relieve these symptoms, even if that treatment is unwanted or disruptive to the patient. Then, if the patient fails to follow those instructions, they are labeled as non-adherent and can feel shame at their inability to “do the right thing” to feel better.
However, by integrating Eastern-medicine practices, we recognize the body’s symptoms as signals that the body is off balance. Then, we can focus on identifying the root cause of the imbalance and associated symptoms, rather than just treating symptoms or waiting for disease(s) to develop and be diagnosed.
Let me give you an example. In Western medicine, we identify and diagnose type-2 diabetes based on blood work demonstrating elevated blood glucose. Then, we treat type-2 diabetes with medications and diet recommendations to bring the blood sugars down. By not treating the root cause, this treatment acts only as a bandaid. It doesn’t solve the problem. In fact, by only focusing on the blood sugars, there is no expectation of reversing disease processes. It is expected that the disease is chronic and progressive and the patient will be on more and more medications for life.
In Eastern medicine, without checking the blood sugars and before the diagnosis of type-2 diabetes, the increasing waist circumference and weight, the fatigue, and/or the fungal infection would be recognized as a body out of balance. The Eastern-medicine practitioner would provide instructions to address the imbalance. The individual would be instructed to practice fasting, acupuncture, tai chi, walking, meditation, and getting restful sleep or nature exposure to “treat” the reason for the imbalance. Treatment efficacy would be monitored by improvements in waist circumference, weight, fatigue, and improvement of the infection.
In Western medicine, we wait until there is an actual diagnosis before we treat. In Eastern medicine, we would treat when the person is reporting something that feels abnormal. In Western medicine, we wouldn’t treat until it had already progressed to a disease state. In Eastern medicine, we would treat when the body first shows it is out of balance and the disease may not even develop.
In the case of diabetes, overweight, and obesity, when Eastern and Western medicine are integrated, we can know that the first signs of an imbalance, such as weight gain around the waistline, are due to an insulin-resistant state, before there is a diagnosis of diabetes. In Western medicine, the diagnosis of type-2 diabetes represents a more advanced state of insulin resistance.
Instead of immediately prescribing medication (Western medicine), which inherently comes with the risk of side effects and other complications, we could improve symptoms by integrating lifestyle behaviors that reduce insulin, stabilize blood sugar, and manage the stress-hormone cortisol (Eastern medicine). Then, adding medications (Western medicine) when necessary to these foundational lifestyle behaviors (Eastern medicine), like fasting, would result in the best outcomes for gaining health.
If you’re experiencing a negative health symptom and your healthcare provider isn’t sharing a variety of Eastern and Western medicine options, spend some time exploring a comprehensive range of modalities, including acupuncture, herbal medicine, dietary therapy, diagnostic tests, and maybe even pharmaceutical interventions or surgery. With the right support, these can be blended and tailored to suit your individual needs and preferences.
Conclusion: It’s Not Eastern versus Western Medicine, It’s Eastern and Western Medicine
Eastern and Western medicine don’t need to be viewed as opposites; in fact, they’re very complementary. We can integrate Eastern and Western medicine and have the best of both worlds. Viewing these two approaches as two halves of a single wellness plan will lead to optimal outcomes for health and longevity. Through the use of Western medicine’s effective screenings, vaccines, antibiotics, and other advanced interventions that effectively treat diseases, you can be spared much suffering and premature death. Then, by integrating Eastern-medicine practices that promote physical movement, meditation, nutrition, restful sleep, and fasting, you can honor your natural rhythms and optimize your lifestyle behaviors to gain health and improve your quality of life.
- Q&A with Dr. P: Weight Management Tips & Tricks - June 6, 2024
- Q&A with Dr. P: Weight-Loss Plateaus, Fasting Metabolism, and More - April 22, 2024
- Bridging the Gap: Eastern and Western Medicine in Modern Times - March 11, 2024