Written and medically reviewed by Nicole Grant, RD
While it may be best known for its role in diabetes, insulin is integral to overall health and weight loss. It plays a dynamic role in regulating not just blood sugar but also your body’s metabolism and energy storage.
Read on to discover how to manage your insulin levels so you can achieve optimal health and a weight that is right for you — with special help from our Chief Medical Officer, Dr. Naomi Parrella!
What Is Insulin?
“Your body has a powerful defense mechanism against high levels of sugar. That defense comes from your pancreas, which pumps out insulin every time your blood-glucose levels skyrocket.”
- Dr. Naomi Parrella
Insulin is a hormone your body produces to manage blood sugar and help regulate what your body does with carbohydrates, proteins, and fats. Insulin release is primarily triggered by an increase in blood-glucose levels, which typically happens when you consume carbohydrate-rich foods. When the pancreas detects high glucose in the bloodstream, it signals certain cells (called beta cells) to secrete insulin. Insulin then directs glucose out of the blood stream and into your body’s cells, particularly muscle and fat cells. It also prompts the liver to store excess glucose.
In addition to its role in glucose metabolism, insulin is instrumental in fat and protein metabolism. It inhibits the breakdown of fats, thereby promoting fat storage — which, to some degree, you need to survive! Insulin also plays an important role in muscle growth and repair by promoting the uptake of amino acids (the building blocks of proteins) into muscle cells. This action is vital for muscle recovery and growth, as it enhances the synthesis of new proteins and prevents muscle breakdown.
Clearly, insulin is a crucial hormone for survival, as it regulates blood-sugar levels and enables cells to use fuel for energy and growth. However, consistently high levels of insulin can lead to weight gain and insulin resistance, disrupting the body’s natural balance and negatively impacting overall health. Therefore, it’s important to find the right rhythms with insulin — stimulating its release when appropriate, but also managing levels so you also don’t chronically have too much.
Does Insulin Affect My Weight-Loss Efforts?
“If you can’t burn sugar, insulin will signal your body to store it. And where do we have infinite storage space? In our fat cells.”
- Dr. Naomi Parrella
Insulin can directly impact your ability to lose or maintain weight. Insulin is considered a growth hormone, meaning that its release in the body triggers the uptake of fuel into your cells to be used as energy or, in the presence of excess calories, be stored in adipose tissue (also known as body fat). Importantly, high levels of insulin can suppress the breakdown of stored fatty acids, making it harder to lose body fat even in the presence of a caloric deficit.
A recent study has shed light on how diets high in glycemic-index (GI) foods can influence weight management, highlighting the role of insulin. High-GI foods, which are known for causing rapid spikes in blood sugar, trigger the body to release more insulin. In the short term, this elevated insulin level can lead to increased fat storage, making immediate weight-loss efforts more challenging. Participants in the study who consumed a diet higher in carbohydrates, especially those rich in high-GI foods, not only gained more weight initially but also faced difficulties in maintaining long-term weight loss. This was attributed to an impaired basal fat oxidation rate — i.e., the body’s ability to burn fat at rest — which is crucial for sustained weight management.
The presence or absence of insulin can also affect hunger. Keeping insulin levels low for longer periods of time promotes the formation of ketones, an alternative energy source that has been shown to reduce hunger levels. Feeling less hungry and more satiated throughout the day can help spontaneously reduce or moderate your overall food intake so you are less likely to overeat or consume an excessive amount of calories. Therefore, if you’re trying to lose or maintain your weight, make sure you’re giving your body enough of a break from insulin to keep levels low and enable you to tap into fuels aside from glucose.
What Can I Do to Manage My Insulin Levels?
“Fasting trains your body to bring insulin levels down, and that’s what Zero does. We’re making it easier for you to tap back into the fat-burning potential that your body has been designed for.”
- Dr. Naomi Parrella
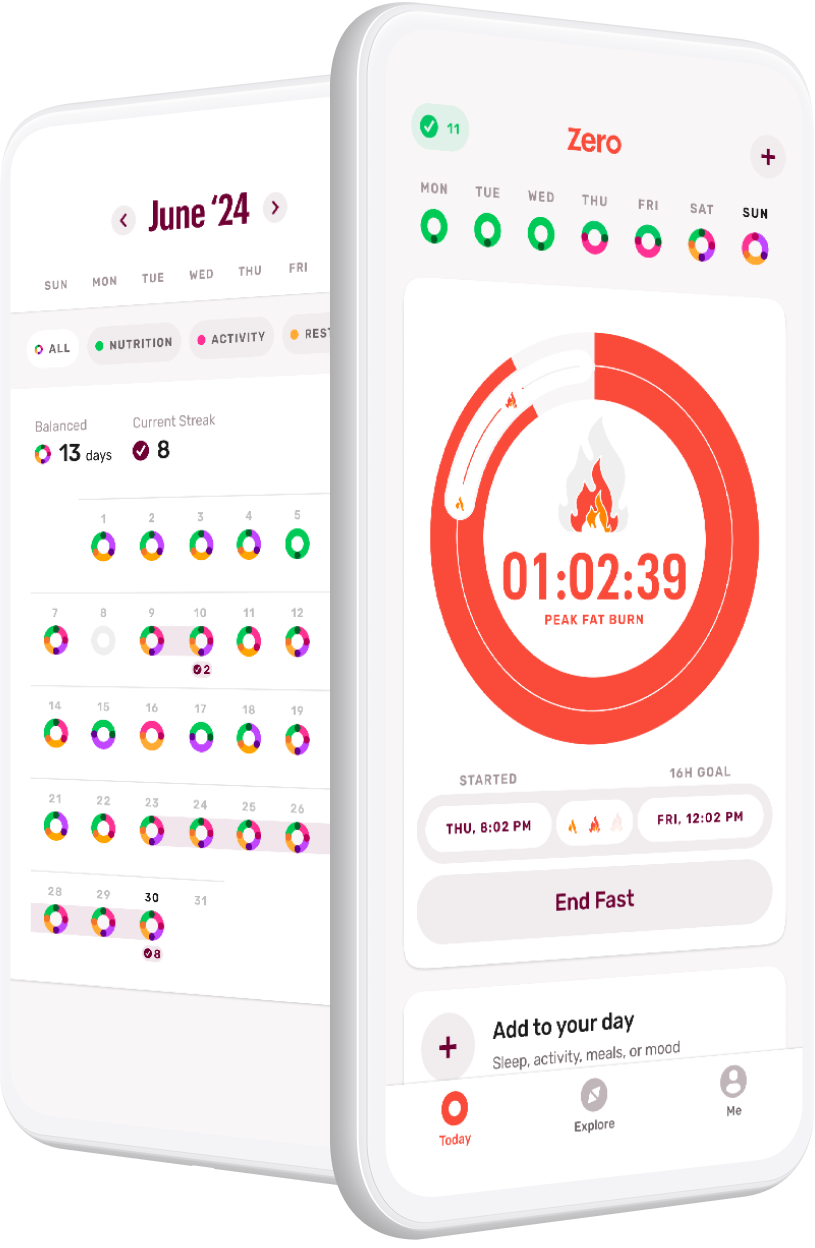
Tip #1: Practice a Consistent Fasting Routine
Intermittent fasting is known to help manage insulin levels. During fasting periods, insulin levels naturally decrease as the body shifts from using primarily glucose from the food you ate to the glucose and fat you have stored in your body for energy. This reduction in insulin is important, as lower insulin levels facilitate fat burning and reduce the likelihood of storing excess calories as fat. For instance, a daily 16-hour fast followed by an 8-hour eating window allows your body ample time in a low-insulin state, thereby increasing your reliance on stored fat for energy and promoting weight loss.
A consistent fasting practice can also help manage certain metabolic disorders, such as insulin resistance. Especially in people who struggle to regulate their blood sugar, intermittent fasting can reduce fasting insulin levels and improve insulin sensitivity. As insulin sensitivity improves, your body naturally releases less insulin. As a result, insulin levels decrease and your body spends less time in an insulin-elevated state, meaning more opportunities for fat loss.
The typical American diet is full of processed, high-GI carbohydrates. Additionally, adults who fall within the overweight and obese categories have been found to eat for 14 hours a day or more, which leaves them with only 10 hours (or less!) of fasting — often resulting in elevated insulin levels for most of their waking hours. To give your body a break from consistently elevated insulin levels, aim to lengthen your daily fasts to 12–18 hours, giving you a 6–12-hour eating window most, if not all, days of the week.
Tip #2: Exercise!
Physical activity is another powerful tool for managing insulin levels. During exercise, your body uses a mix of glucose and fatty acids to fuel movement. If you’re doing fasted exercise, your glucose and insulin levels will likely already be lowered, so working out will help you maintain those levels. If you’re exercising during your eating window, your body will pull the glucose from your blood to use as fuel, lowering total blood glucose and decreasing the need for excess insulin.
As an added benefit, exercise can have positive effects on blood glucose and insulin long after the exercise is done. Studies have shown that cells continue to suck up glucose at an accelerated rate for up to 2 hours after exercise, and insulin sensitivity can be improved for up to 16 hours in both healthy and diabetic populations.
Any movement is good movement, so aim for a blend of zone 2, strength training, and high-intensity exercise to help optimize insulin levels. Zone-2 movement, such as a brisk walk or light bike ride, can improve your overall metabolic flexibility, which helps your body more easily switch between using glucose and fat for fuel. Strength or resistance training helps increase your muscle mass, essentially creating more space for glucose in the muscle so that excess glucose doesn’t get dumped into the blood. Finally, high-intensity training, i.e., exercising at >80% of your maximum heart rate, uses glucose as your primary fuel, which can help you more rapidly use up any excess glucose in your blood and consequently lower insulin levels.
Tip #3: Be Wise About Your Carbohydrates
The type and amount of carbohydrates you consume play a significant role in managing insulin levels. To help keep insulin levels low, aim for moderate-to-small portions of carbohydrates in your meals, especially the meal right before you start your fast.
Also, opt for minimally processed carbohydrates. These are foods typically found in their whole form — vegetables, fruits, legumes, whole grains, and dairy. The more minimally processed carbohydrates tend to have a lower glycemic index and glycemic load, which causes a slower, more gradual rise in blood sugar and, consequently, less insulin release. On the other hand, high-glycemic foods like white bread, pastries, and sugary drinks should be consumed sparingly, as they lead to rapid spikes in blood sugar and insulin.
Finally, balance your carbohydrate intake with adequate fiber and healthy fats. Eating this combination of nutrients can help slow down the absorption of glucose into your bloodstream and mitigate insulin spikes.
Conclusion: If You Want to Manage Your Weight, First Mange Your Insulin
Insulin is key to mastering your metabolic health and succeeding at healthy, sustainable weight loss. Insulin’s intricate involvement in your body’s energy use and storage demonstrates how interconnected your fasting practices, dietary choices, and exercise habits are to your well-being. Whether it’s adopting a consistent 12–18-hour fasting routine, engaging in regular physical activity, or making wise carbohydrate choices (or a combination of all three!), each step you take can significantly influence your insulin levels and, in turn, lead to weight loss and health gain. Start your journey towards better insulin management today, and make progress towards your health and weight-loss goals.
- 4 Easy Tips to Burn Fat Faster - July 3, 2024
- Why Should We Care About Hormones? Fasting and Hormone Health - April 1, 2024
- Should You Consider a Continuous Glucose Monitor (CGM) If You’re Non-Diabetic? - March 18, 2024