Written and medically reviewed by Katya Meyers, RD
You’ve likely heard of intermittent fasting, even if you have yet to try it for yourself. Many advocates tout fasting’s weight-loss, insulin-management, metabolic-health, and other anti-aging health benefits. While these effects can benefit both men and women, intermittent fasting may be an especially useful dietary strategy for women suffering from polycystic ovary syndrome (commonly known as PCOS). Intermittent fasting for PCOS can reduce symptoms and improve fertility and other quality-of-life outcomes.
What Is PCOS?
Polycystic ovarian syndrome is a hormonal irregularity that affects as many as 10% of women worldwide. It is characterized by small cysts that develop on the ovarian follicles when ovulation does not occur. These cysts produce androgens (male sex hormones), which may further contribute to menstrual dysfunction and loss of ovulation.
However, it is important to note that the cysts are not the cause of PCOS, but a symptom. The exact cause of PCOS is not well understood, in part because it is likely influenced by many factors. It may stem from genetic, environmental, and behavioral causes. Women who have mothers or sisters with PCOS are more likely to suffer from it, as are women who have poor insulin sensitivity and are overweight or obese. Exposure to environmental toxins may even play a role.
The most common PCOS symptoms include: missed or irregular periods, ovarian cysts, hirsutism (excess body hair), weight gain (particularly abdominal weight gain), acne, and male-pattern baldness. In addition, PCOS is a primary cause of infertility in women of childbearing age. However, not all women with PCOS may have all symptoms or risk factors, making it difficult to diagnose. Most women who have PCOS do not know they have this common reproductive endocrine disorder.
What Is Intermittent Fasting for PCOS?
A research-backed PCOS diet has not yet been established. However, because increases in weight and blood sugar levels can increase the risk of PCOS and worsen symptoms, clinicians have recommended a number of dietary and lifestyle changes. (Up to 1 in 4 women diagnosed with PCOS can become obese, so early and effective intervention is necessary.)
Intermittent fasting may be one way to reduce your chances of acquiring PCOS and other obesity-related diseases, including cardiovascular disease and metabolic syndrome. Moreover, if you already have PCOS, intermittent fasting may help improve your symptoms.
Is Intermittent Fasting Good for PCOS?
While no one “best diet” for PCOS has been identified, research shows that following a healthy diet can improve symptoms of PCOS and dramatically improve your cardiometabolic health. The key is therefore to identify a healthy diet that women can stick to.
There is overwhelming evidence that a nutrient-dense diet — one that is high in fruits, vegetables, high-quality proteins, and healthy fats — has copious long-term health benefits. Yet, it’s also clear that people find it difficult to stick to a consistent plan of eating. A calorically restrictive diet paired with exercise can improve symptoms of PCOS, but this regimen has proven difficult to follow in the long term.
Instead, an intermittent-fasting approach may deliver an effective and realistic way to symptom management. Intermittent fasting does not attempt to constrain what or how much you eat, only when you eat. Studies have shown that following an intermittent-fasting program can be easier than other types of diets because it results in lower hunger levels than typical diets involving caloric restriction, while still spontaneously creating a caloric deficit.
Adherence aside, there are numerous health benefits of intermittent fasting. What makes intermittent fasting an especially good fit for women suffering from PCOS is its ability to improve biomarkers such as body weight, body-mass index, blood-glucose levels, and insulin levels, all of which can help you manage PCOS.
How Intermittent Fasting Affects Hormone Levels
The majority of women with PCOS have insulin resistance, even if they are not overweight. Being insulin resistant means that your body’s cells do not respond to the effects of insulin, which ordinarily helps your cells absorb glucose from your bloodstream. As a result, blood sugar levels remain high, to which the human body responds by releasing even more insulin. High levels of blood glucose and insulin can result in serious health problems such as type 2 diabetes and heart disease; therefore, early and effective intervention is necessary.
Unfortunately, high insulin levels are not just a symptom of PCOS — they’re also a major driver of the condition. High insulin levels can impair ovulation and cause the ovaries to make excess testosterone, which can increase the risk of menstrual-cycle dysfunction and exacerbate symptoms.
Regularly allowing your body to spend time in the fasted state through intermittent fasting improves glucose regulation and insulin sensitivity. Intermittent fasting allows your body to switch into more of a “fat-burning mode” where you rely on your own body’s fatty acids and ketones for fuel, as opposed to glucose from the carbohydrates you consume. Flipping this metabolic switch can improve glucose regulation and insulin sensitivity, leading to improvements in PCOS symptoms, and lower risk of other metabolic diseases, such as type 2 diabetes.
The Science Behind Intermittent Fasting and PCOS
While more human studies directly examining the effects of intermittent fasting on PCOS are needed, one six-week trial of females with PCOS showed that restricting food to an 8-hour eating window led to significant improvements in PCOS symptoms and markers, including a reduction in weight, body fat, and androgen levels. In addition, following this diet for six weeks improved markers of chronic inflammation and restored normal menstrual function for 73% of women in the study.
Another study done in mice with PCOS examined the effects of intermittent fasting on endocrine function. After intermittent fasting for 8 weeks, the mice showed significant weight loss, fat loss, and improved glucose control. These changes helped to lower the mice’s abnormally high androgen, luteinizing hormone (LH), and follicle-stimulating hormone (FSH) levels (all caused by PCOS), resulting in improved reproductive function.
PCOS Intermittent Fasting for Weight Loss
In addition to regulating hormones, intermittent fasting for PCOS can also lead to weight loss. Though not everyone with PCOS is overweight, one longitudinal study showed that women with PCOS are up to four times more likely to become overweight or obese. Research shows that, in the general population, intermittent fasting is at least as effective at creating weight loss as calorie restriction and can provide additional health benefits, such as improved glucose control. In short, intermittent fasting for PCOS can help you live a longer and healthier life.
The Best Intermittent Fasting Schedule for PCOS
Regardless of the type of intermittent fasting that’s right for you — whether it’s time-restricted feeding, alternate-day fasting, the “5:2,” or something else — IF works by simply condensing your eating period in different ways. One of the most common methods is to shorten your eating window each day, a strategy known as time-restricted feeding, or TRF.
For example, a 16:8 pattern means you fast for 16 hours and eat your food within an 8-hour window of time. You might do this by delaying or skipping breakfast or by eating an early dinner and forgoing late-night snacks. While by definition intermittent fasting means that you spend more time in the fasted state, the good news is that you can choose a period of time that is easily integrated into your normal day. Love having breakfast with your partner who often works late? Choose an earlier eating window. Or, if family dinners are the thing you just can’t do without, wait a few hours before having breakfast so that your first meal falls later in the day and your fasting window extends into the evening.
Alternatively, you may find that fasting is not something you want to do every day, but you still want the benefits of intermittent fasting for PCOS. Some people find that alternate-day fasting (ADF) to be effective. In ADF, you toggle between one day of ad libitum (“normal”) eating and one day of either ordinary fasting or modified fasting where you lower your caloric intake by ~25% of your normal daily needs. (This latter option is typically intended for weight loss, so if that’s not your goal, stick to a gentler fast where you eat your full caloric allotment for the day.)
Whichever intermittent fasting schedule you choose, the most important part of your intermittent fasting plan is consistency. However, a growing body of research indicates that at least some of the positive effects of TRF stem from aligning your food intake with your circadian rhythm. A typical circadian rhythm controls wakefulness across a 24-hour day. Late-night snacking can disrupt this natural rhythm, which can cause problems with sleep and healthy metabolic function. Aim to align your eating with daylight hours as much as possible, and end your eating window 2–4 hours before bed.
How to Start Intermittent Fasting for PCOS
Now that you’re clear on the different methods of intermittent fasting for PCOS, the next step is to simply begin — but do it gradually! Even if you’re feeling highly motivated, the best way to start your fasting habit is to take it slow. Though beneficial, fasting is a form of stress to your body. Building your tolerance for fasting over time — just like you would exercise — gives your body time to adapt and is likely to increase your adherence in the long term. Instead of beginning by jumping into longer fasts right away, ease into it.
Is Intermittent Fasting Safe for Everyone with PCOS?
For most women with PCOS, intermittent fasting can be a safe and effective part of your health journey. However, there may be some women for whom intermittent fasting for PCOS is not the right approach . If you have any of the following conditions, intermittent fasting may not be right for you at this time:
- You are pregnant or nursing
- You have been diagnosed with a past or current eating disorder
- You have type 1 or type 2 diabetes, are taking medication, or are managing another health condition
As with any change you’re considering in your health routine, be sure to consult with your doctor.
Conclusion
As with most diet and lifestyle changes, there is no one-size-fits-all approach. Ultimately, only you can decide if intermittent fasting is right for you. However, given the research, there is little doubt that for some women, intermittent fasting for PCOS can help improve symptoms.
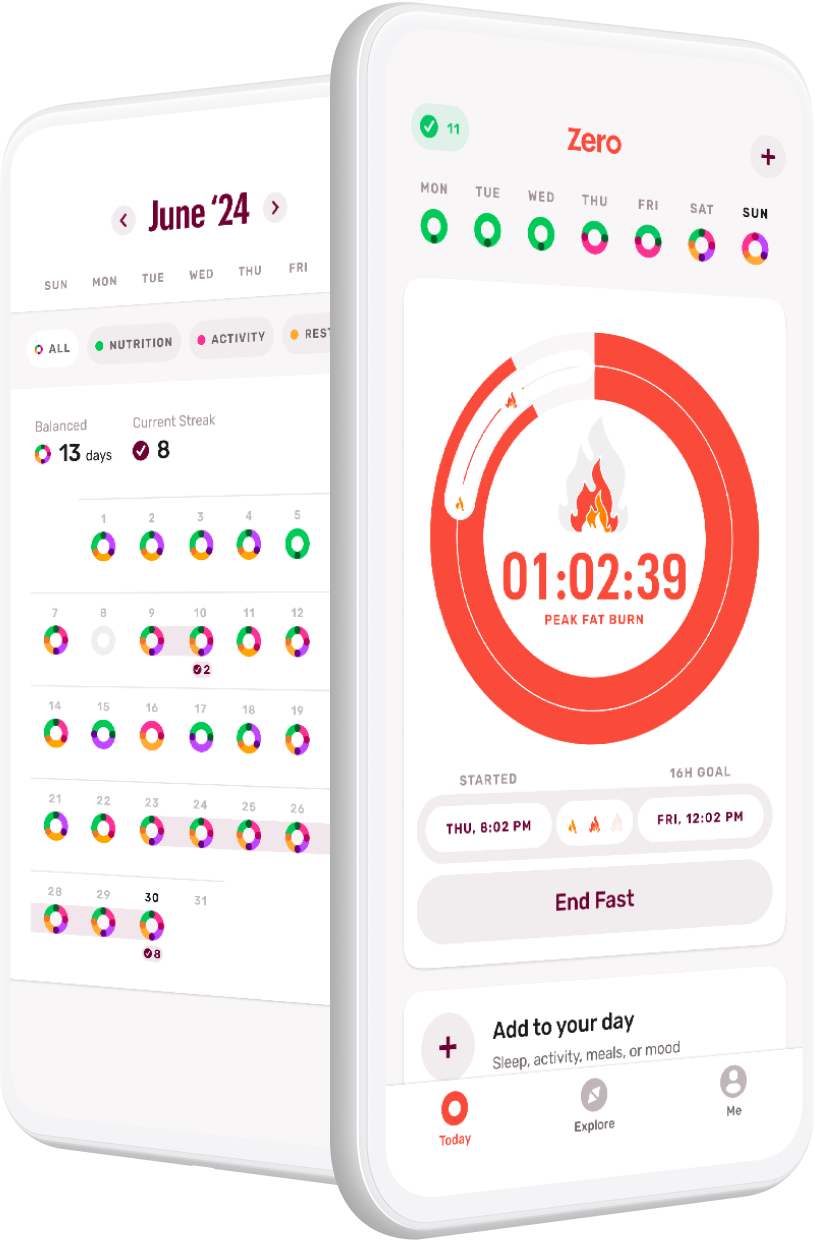
Ready to start using Zero? Take the quiz or download the app today.
- The Fasting Guide to Menopause, Perimenopause, and Postmenopause - April 8, 2024
- Try This Instead of That: How to Bookend Your Fasts - March 25, 2024
- 60 Names for Sugar: The Myths, The Facts, and What You Should Know - February 12, 2024