As interviewed by Rich LaFountain, PhD
We are thrilled to introduce Dr. Naomi Parrella as Zero’s Chief Medical Officer!
Dr. Parrella is a renowned physician who has spent decades treating patients and educating both medical students and the broader public about obesity and metabolic health. Dr. Parrella spent her formative years in Japan before coming to the United States for high school, college, and, eventually, medical school. These experiences ultimately led her to blend Eastern and Western medicine in her efforts to help patients from all backgrounds and walks of life.
In addition to working directly with thousands of patients in her medical practice, Dr. Parrella is a highly sought-after speaker and expert consultant collaborating with organizations including the NFL, United Airlines, and Google. She pursues opportunities to engage with the public outside of her medical practice because she is on a mission to share the knowledge and wisdom she has gained with as many people as possible. This was one of her key motivators for joining Zero.
Q&A with Dr. Parrella
Q: We are thrilled to have you join Zero as our Chief Medical Officer. What excites you most about your role in supporting Zero’s mission?
A: As a family physician and obesity-medicine specialist, I have seen firsthand all the ways unhealthy weight can aggravate health problems and interfere with people’s freedom to live their best life. I have also seen that it doesn’t have to be that way. By understanding and tapping into our body’s natural capacity to heal, regenerate, and thrive, we can often prevent, reverse, or at least improve some of these problems. Zero is an ideal tool to do this.
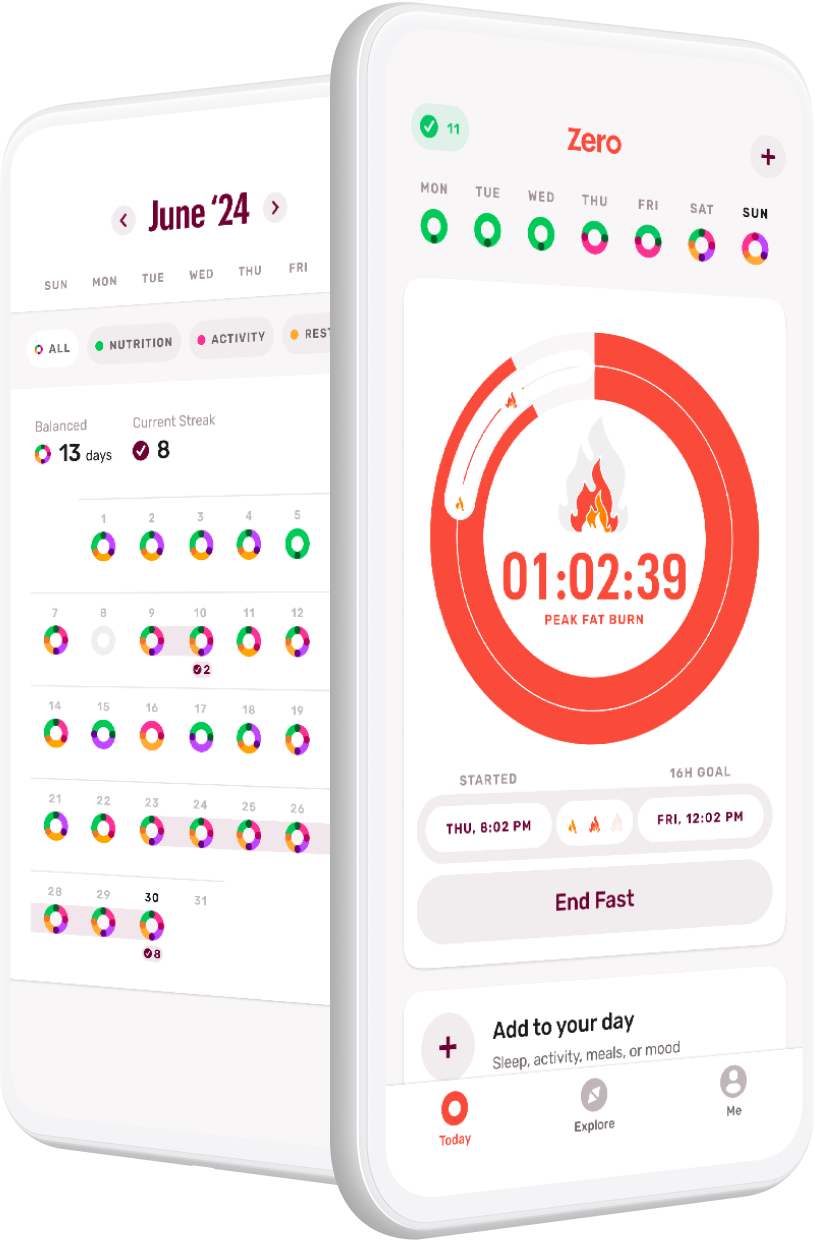
In fact, I’ve already been using Zero with my patients for quite a while! The app provides support and coaching for my patients during all those hours they are not in my office. Plus, it makes it possible for their friends and family, who can’t come to my office, to still join in on their weight-loss and health journey. Especially now, with Fat-Burning Mode and so many great ways to link fasting with other healthy behaviors, you can get a holistic picture of the habits that are helping or hindering your body’s natural fat burning.
This is something I’m always trying to do with patients. After we cover the relationship between fat burning and insulin — when insulin goes up, fat burning goes down — we work together to develop habits that will keep them in a state of fat burning longer. I usually recommend starting with shorter fasts of 12 hours, which can help to reduce insulin. Then, if people want to lose weight and improve their metabolic health, we may find that extending their fasts slightly, to 14 or 16 hours, boosts progress. Or, they may find other fasting patterns that work better for their job, school, or home schedules. Some days, they may choose not to fast, so they need a plan for that. In other words, there are many different ways to fast, and some are more effective for an individual than others. The key is finding the pattern(s) that work best for you and your body, in your life, and knowing how to best break your fasts to get the best results.
Zero is giving all of these options and the same guidance I provide, but at a much bigger scale to benefit many more people. I’m really excited about helping many more people flip the metabolic switch the way I help individual patients in 1:1 appointments.
Q: What drives you to invest so much of your time and energy in sharing your knowledge about weight loss and metabolic health outside of your clinical practice?
A: If I can see 100 patients in a week and several thousand across a year’s time, that’s great. But the message should go beyond those individuals. So, if somebody comes to me and says, “Hey, would you like to talk to this larger group and share a message that could help them?” I say, “Bring it on!” If a company is interested in helping their employees thrive, I’m in. If a group like the NFL wants help going out to elementary schools and getting kids excited about physical activity, sign me up. I’m all about spreading the message and letting people see it’s actually possible to feel better and do better. It’s exactly why I jumped at this opportunity to partner with Zero.
Q: Considering your extensive work helping people gain metabolic health and combat obesity, what do you see as a common obstacle for patients? How do you support your patients in overcoming these barriers?
A: The most common challenge I see patients face is frustration, with maybe a touch of confusion based on common, well-intended misinformation. The loudest, most publicized headline information they receive seems to change or, worse, contradict previously established knowledge all the time. And remember: Many people who have tried to lose weight have had some success in the past. However, they often report they regained the weight, or they had minimal success that was not worth the effort, and they are tired of disappointments and feeling like they failed.
I help patients overcome frustration by teaching them about fat burning. Often, I draw a little chart. Your body can be in a state where it readily burns fat, or it can be in a state where fat burning is blocked. Many people default into a lifestyle and dietary pattern that reduces the time they spend in a fat-burning state. This can make it challenging to maintain a healthy body weight and metabolic health in the long term. The good news is that, with the right guidance, this can be improved.
Q: How does someone get into a fat-burning state, and how does that contribute to weight loss?
A: It’s a metabolic fact that if your insulin is high, your ability to burn fat is undermined. Insulin is a potent inhibitor of lipolysis (a.k.a. fat burning), so when insulin levels are high your body cannot reach its true fat-burning potential. In order to burn more fat, you need to engage in behaviors (like using Zero!) and make dietary decisions that will bring your insulin levels closer to a natural baseline. In a low-insulin environment, your body can naturally burn fat for fuel, which is what healthy weight loss is all about.
Knowledge empowers. I find that when people better understand what habits block fat burning and what habits improve it, they often make lifestyle choices that improve their metabolic function, which can lead to their desired weight loss. For example, sugar, processed and starchy carbohydrates, and even some artificial sweeteners can spike up insulin levels. When insulin spikes up, fat burning stops. Knowing how to use this information, for example, how to best manage this during birthdays and celebrations, can limit frustration when weight-loss challenges surface.
If you want to facilitate fat burning, fasting is key. After 12 or more hours (for each person, the number of hours may be different), your body will “flip the metabolic switch” and start to burn fat. If you want to speed up that process, you might prioritize eating more protein, fibrous veggies, and/or naturally occurring fats. You may also choose to take a walk, swim, or bike ride.
When your body is in fat-burning mode, it has access to your largest source of energy — your stored fat, which has on the order of tens or hundreds of thousands of calories of fuel. With that ready supply of fuel, you may not feel the need to eat or snack between meals. As a result, you might find yourself not being as hungry, not eating as much, and not depriving yourself. And you will be burning that extra fat stored in the body. Win-win.
Q: How does intermittent fasting fit within the diverse landscape of obesity treatments and your fat-burning model?
A: Intermittent fasting is a very important strategy for obesity, and it clicks right into the fat-burning model. Fasting for 12 or more hours is a great way to flip the metabolic switch so that you can be in a fat-burning state. We know that fasting for roughly 12 hours brings insulin down, though some people require longer.
In addition to fasting, exercise or general physical activity — just how you move during your normal daily activities — can promote metabolic switching. In fact, people who are more active throughout the day often have an easier time flipping the switch. The same goes for people who do a good job managing stress and prioritizing sleep — studies show they often have greater metabolic function and health.
Ideally, you want metabolic flexibility, or the ability to easily switch in and out of fat burning. You don’t need to remain in a fat-burning state all the time; your body wants choices. For example, during short bursts of intense exercise, your body may choose to burn sugars like glucose or glycogen because those fuels provide more rapid energy. However, if you keep working out, your body may need more fuel, and it helps to be able to tap into the fat cells for more fuel. I enjoy helping people discover simple tweaks to their habits so that they can get the benefits associated with fat burning.
Q: How has your philosophy changed throughout your career regarding nutrition and lifestyle medicine?
A: Early in my career I believed that weight loss was simple — you just had to teach people to “make the math work” with calories and energy expenditure, a.k.a. “calories in, calories out.” As my career progressed, however, I came to see that it just didn’t work for most people I worked with, and there’s more than one way the human body can thrive.
My early exposure to Eastern medicine almost certainly influenced this belief. In Japan, for example, when the body has a fever, you may or may not work to bring down body temperature because it might be your body’s immune system effectively fighting it for you. Why stand in the way of that process? When you have a fever in the U.S., however, you typically use medications to bring down the temperature and reduce fever symptoms. Both methods can — and do — work! Your body is capable of tremendous healing.
Today, I try to tailor my recommendations to match patients’ needs and preferences — and their unique circumstances — while still producing real, clinically meaningful results. Of course, sometimes patients don’t follow my recommendations and try something different… and sometimes they still get better! I’m pleased when my recommendations improve their health, but I learn more every time a patient finds success with a strategy or method that’s new to me. The way I see it, it’s an opportunity to expand my repertoire to help future patients.
Q: There is still an active debate about “calories in, calories out” and variations of the carbohydrate-insulin model for obesity. How do you see these theoretical models impacting real patients in everyday life?
A: I was once a believer in the “calories in, calories out” approach. In school and in the subsequent training I received, I was always told that you had to cut calories and, since fat contains the most energy per gram consumed, the way to make calorie restriction easier was to adopt a low-fat diet.
In college, I taught aerobics at a local YMCA. When members of my classes asked how to lose weight, I told them to eat less fat and exercise more. According to the arithmetic, this simple strategy should provide miraculous, sustainable weight loss. But it didn’t take long to recognize it wasn’t working. I had a 100% failure rate for long-term weight loss with the advice I was trained to give.
The wisdom of the day was that when people failed to lose weight following a low-fat, low-calorie diet, they were probably just eating more than they thought and not exercising enough. But here, that wasn’t the case. I saw these people participating in my exercise classes, sweating buckets. Was it possible that everyone was bad at counting calories or flat-out lying about what they ate? I just didn’t believe it. But the one thing I knew was constant with all of them was my advice.
Eventually, I had to rethink everything I had learned. Instead of blaming people for failing to lose weight with advice that wasn’t working, I started looking at weight-loss literature from around the world and exploring different ways of helping people that did not involve forced energy deprivation and exercise. In time, I formed my own practice, and it blossomed because I was listening and looking for opportunities to help rather than handing down an oversimplified, one-size-fits-all solution. The funny thing about caring for patients is that they will tell you when they’re doing well and when they’re not doing well, and the labs speak for themselves. So, if you’re open to it, you get direct feedback, and together with the patient you can work on a solution for managing weight and building health for the long term — usually through a foundation based on lifestyle habits.
Wrap-Up: An Exciting Partnership
Dr. Parrella is an award-winning physician who has deep experience working with patients, educating medical students, residents, and fellows, and sharing information with the broader community on the topics of obesity and metabolic health. We are proud to partner with her to bring about positive change in human healthspan and lifespan.
- The Complete Guide to Fat Burning - April 30, 2024
- Zero Live #4: 3 Ways to Boost Fat Burning - March 28, 2024
- Zero Live #3: Nutrition, Fast Breakers, and Fasting - March 11, 2024